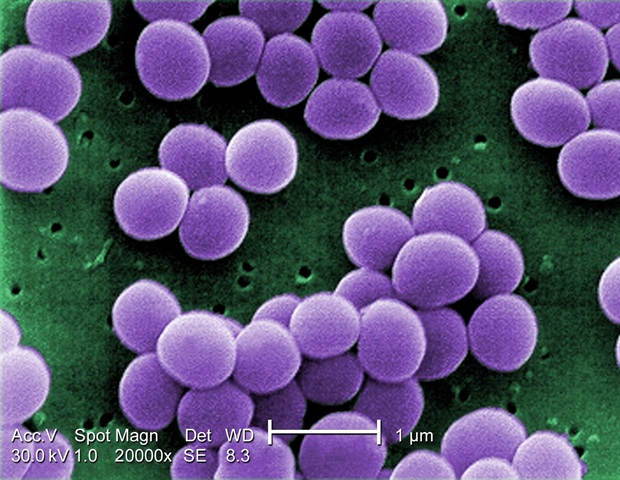
Neonatal intensive care units (NICU) should balance the prevention of Staphylococcus aureus infections in critically ill infants with the need for skin-to-skin contact with parents and siblings, according to a Society for Healthcare Epidemiology of America (SHEA) white paper published in the journal Infection Control & Hospital Epidemiology.
The paper serves as a practical clinical companion to the newly released recommendations from the Centers for Disease Control and Prevention’s (CDC) Healthcare Infection Control Practices Advisory Committee to help clinicians in NICUs make decisions about infection prevention, detection, and control practices.
Infants remain at risk for Staph infections, yet there are effective strategies to decrease transmission that can easily be applied within the NICU without sacrificing the vital benefits these very young, tiny infants receive from care and bonding with parents, caregivers or other close relatives.
Limited literature exists on prevention of Staph in the NICU, so this document looks to address common challenges faced by healthcare personnel in this environment.”
Ibukun Akinboyo, MD, Study Author and Medical Director of Pediatric Infection prevention, Duke University Hospital
The paper, SHEA neonatal intensive care unit (NICU) white paper series: Practical approaches to Staphylococcus aureus disease prevention, provides expert opinion and evidence-based responses to frequently asked questions clinicians may have in implementing the updated CDC guidance for preventing, detecting, and controlling the spread of Staph infections, including methicillin-resistant S. aureus (MRSA) and methicillin-susceptible S. aureus (MSSA).
Staph infections can become serious in NICU patients and are often associated with medical devices, like catheters used for feeding and medication, as well as direct and indirect exposure to bacteria on healthcare personnel, parents, caregivers, family members, other critically ill infants, and the healthcare environment.
The document discusses how to safely handle Staph bacteria colonization and infection in parents or visitors and in NICU patients, including hospitalized multiples (e.g., twins or triplets) with different colonization or infection statuses.
The document can also help guide decisions about when and how to decolonize infants who have asymptomatic S. aureus or MRSA, while taking into account safety considerations for this patient population.
The authors note that recommendations may need to be adjusted during outbreaks of S. aureus or MRSA to address specific issues.
Akinboyo, I. C., et al. (2020) SHEA neonatal intensive care unit (NICU) white paper series: Practical approaches to Staphylococcus aureus disease prevention. Infection Control and Hospital Epidemiology. doi.org/10.1017/ice.2020.51.