Image: Shutterstock
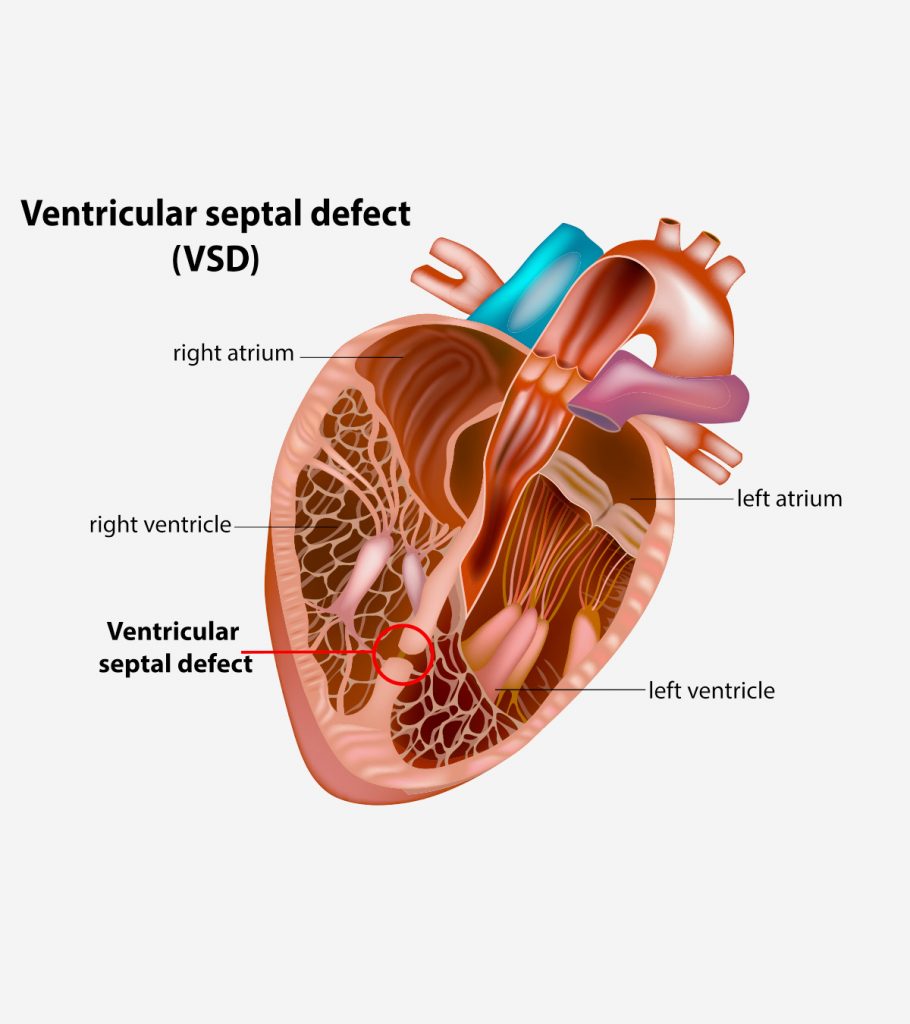
Ventricular septal defect (VSD) is an abnormal opening in the ventricular septum, the tissue or wall that separates the heart’s lower chambers (ventricles). It is one of the most common types of congenital heart defects, accounting for about half of congenital heart disease cases in babies.
The ventricular septum prevents the mixing of oxygenated and deoxygenated blood contained within the left and right ventricle, respectively. Opening in the ventricular septum could allow blood from the left ventricle to reach the right ventricle and lungs. Advanced cases could also display the reverse flow of the blood from the right ventricle to the left ventricle.
The treatment often involves surgical closure of the opening, and it could improve the baby’s condition. Read this post to know about the types, causes, symptoms, diagnosis, treatment, and prevention of ventricular septal defect in babies.
Types Of VSD In Babies
Ventricular septal defects are classified into four basic types based on their location in the heart (1).
- Muscular VSD is the most common type, located in the septum’s muscular portion. This may close naturally in most babies without any surgical interventions.
- Membranous VSD is an opening in the upper part of the ventricular septum, known as a membranous septum, near the valves. This type may not close naturally and often requires surgery to close it.
- Atrioventricular canal type VSD is associated with atrioventricular canal defect. In this type, the defect is located below tricuspid and mitral valves, which are valves between the upper chambers (atria) and lower chambers (ventricles) of the heart.
- Conalseptal VSD is rare and occurs below the pulmonary valve, the valve between the right ventricle and pulmonary artery leading to the lungs.
Causes And Risk Factors For VSD
VSD is a congenital heart defect, which means it is present at birth. The fetal heart development begins as a hollow tube and is later divided into four chambers. VSD could occur due to fetal heart development problems during the first eight weeks of pregnancy.
Genetic factors, such as chromosomal abnormalities, or environmental factors, such as exposure to teratogens, may interfere with the heart’s normal partition, leaving an opening in the ventricular septum (2).
Babies with a positive family history of VSD and Down’s syndrome may have an increased risk of developing VSD. In some cases, there may be no discernible cause or risk factor associated with VSD.
Signs And Symptoms Of VSD
Signs and symptoms may vary based on the size of the defect and the baby’s age. The ventricular septal defect allows blood from the left ventricle to reach the right ventricle. This may increase the work of the right ventricle and the lungs. If the hole is larger, more blood enters the heart’s right side, causing severe symptoms.
The following signs and symptoms are seen in infants with VSD (3).
- Additional blood reaching the lungs may cause congestion and rapid or heavy breathing
- Fatigue
- Sweating
- Refusal to feed
- Pale skin
- Rapid heart rate
- Poor weight gain
These symptoms and signs may also be seen in more severe congenital heart diseases. You may consult the pediatrician for early diagnosis and treatment.
Complications Of VSD
Small-size VSD may not cause any complications. Mild to life-threatening complications are often seen in babies with large and medium-size defects. These complications may include (4):
- Pulmonary hypertension (high blood pressure in the lungs’ blood vessels) can be seen in VSD due to excess blood flow to the lungs.
- Heart failure may occur in some babies since the lungs have too much blood and the heart has to work harder to pump blood.
- Endocarditis is the inflammation of the heart’s inner lining (endocardium).
- Valve failures and rhythm abnormalities may occur due to abnormal blood flow in the heart.
- Eisenmenger’s syndrome occurs in babies with severe VSD with pulmonary hypertension. This is a condition in which the direction of shunting reverses, which means the blood from the right ventricle (deoxygenated blood) begins to reach the left ventricle due to pulmonary hypertension. This may cause cyanosis in babies.
Cyanosis in a baby with previous VSD symptoms may indicate Eisenmenger’s syndrome (reversal of blood flow). You may seek immediate medical care since this may increase the risk of complications, such as cerebrovascular accidents, hemoptysis (coughing up blood), and syncope (loss of consciousness).
Prevention Of VSD In Babies
Prevention may not be possible in most cases. However, the following pregnancy care may reduce the risk for VSD in some babies (5).
- Preconception and early prenatal care may help the mother begin a healthy lifestyle and diet before fetal heart
- Seek prescriptions before taking medications in pregnancy to prevent fetal damage due to certain medicines.
- A balanced diet with recommended vitamins (including folic acid) and iron supplements helps the fetus’ optimal growth.
- Regular exercise during pregnancy may also be beneficial for the fetus.
- Vaccination may reduce the risk of congenital defects due to infections.
- Maternal diabetic control during pregnancy may reduce the risk of heart problems in babies.
- Avoid illegal drugs, alcohol, and tobacco products during pregnancy.
If you or your partner has a family history of VSD or other genetic defects, seek genetic counseling, especially before conception.
Diagnosis Of VSD
Signs and symptoms are often suggestive of VSD in some babies. Doctors may hear heart murmurs using a stethoscope during the physical examination of babies with VSD.
The following tests are often done to diagnose the presence, size, location, and complications of the VSD in babies (6).
- An echocardiogram helps determine the size, severity, and location of the VSD and other heart A fetal echocardiogram may allow diagnosis before birth.
- Chest X-ray may help look for the heart’s size (cardiac enlargement) and excess fluid in the lungs.
- Electrocardiogram or ECG may help identify rhythm abnormalities by recording the heart’s electrical activity.
- Pulse oximetry could determine the blood’s oxygen levels. Shunting of blood may reduce the blood’s oxygen levels.
- Cardiac catheterization by inserting a catheter (thin, flexible tube) through the arm’s or groin’s blood vessels could help assess the heart’s structure and function.
Babies with genetic abnormalities may require genetic testing to identify the abnormality. Doctors may plan the interventions based on the diagnostic results.
Treatment Of VSD In Babies
Small-size defects may not need surgical repair in most cases. Doctors may observe for symptoms and wait for the opening to close independently. However, small openings near the heart valves require surgical closure to prevent complications.
Medium and large VSD may require surgical repair within the first year of life. Treatment for VSD may include the following interventions (7).
- Open heart surgery is done to close the opening with stitches or patches. General anesthesia is needed for this procedure, and babies are supported with a heart-lung machine.
- The catheter procedure uses a special mesh device to close the opening without a chest incision.
- Extra nutrition is prescribed for babies who are tired during feeding or unable to feed themselves due to VSD to meet optimal growth.
- Medications, such as diuretics (furosemide/Lasix), are often prescribed to reduce the blood circulation in the lungs.
The type of procedure is chosen based on the size of the opening and babies health status. You may talk with the pediatric cardiac surgeon or cardiologist to know the best treatment option for your baby. Your baby may require several follow-up visits after the surgery to ensure improvement. Long-term prognosis may depend on the type of VSD and its severity, and adequate lifestyle management may help improve the outcome in the long run.