Since the onset of the coronavirus disease 2019 (COVID-19) pandemic, caused by the severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2), millions of people have died, with well over a hundred million infections having been reported worldwide. Some groups are especially vulnerable to the virus, developing severe and progressive disease.
The World Health Organization has identified pregnancy as a high-risk group for COVID-19, especially in pre-existing medical conditions, advanced maternal age, and a high body mass index (BMI). The primary adverse outcomes include more severe disease and preterm birth.
Population-based studies are essential to gain knowledge of the spread and management of this disease. However, most studies on pregnancy during COVID-19 have not been broadly applicable to Nordic populations, like most current COVID-19 research in general.
A new study, appearing on the preprint medRxiv* server, focuses on pregnancies in these countries alone to derive conclusions regarding the association of these conditions.
In Nordic countries, the population composition is far more uniform than in most developed countries, while healthcare in pregnancy is free. All pregnancies and their outcomes are also recorded in medical birth registries. This homogeneous and well-cared-for group of pregnancies is thus separately assessed in the current population-based study.
Characteristics and risk factors
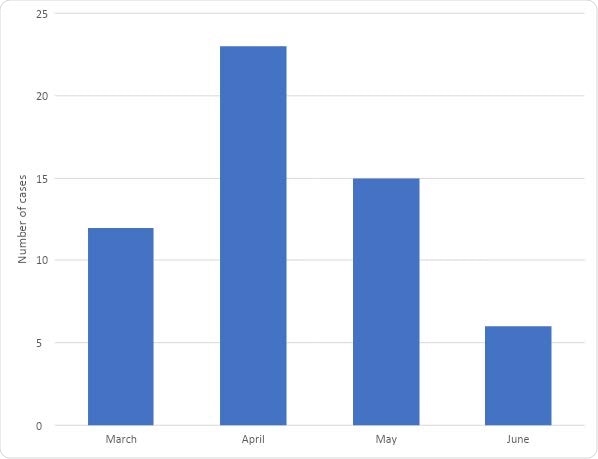
From March to June 2020 (both months inclusive), there were 214 admissions of pregnant women diagnosed with COVID-19. The diagnosis was based on a positive RT-PCR (reverse transcriptase-polymerase chain reaction) within 14 days of admission. The rate of admission varied widely, from less than 1 per 1,000 deliveries in most Nordic countries to above 18 per 1,000 in Sweden.
Since all of these admissions were not due to COVID-19 per se, the remaining analyses were carried out on the subset of 56 pregnant women who required admission only because of COVID-19.
The three Swedish hospitals in this study contribute about a fifth of the total number of births in this country, which allows for significant under-reporting of COVID-19- related admissions and outcomes. Additionally, the cases reported from these university hospitals could suffer from selection bias.
In this group, hospital admission rates ranging from 0.3 to 0.5 per 1,000 deliveries in most Nordic countries to almost 4 per 1,000 in Sweden. No hospitalization cases in pregnancy due to COVID-19 were reported from Iceland over the first four months of the pandemic.
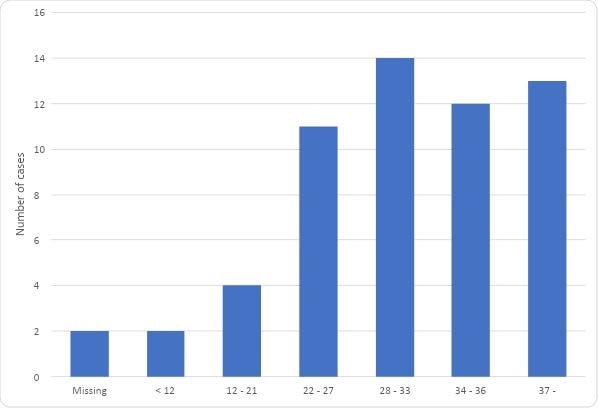
Most women admitted due to the infection in pregnancy were in their third trimester when they received the diagnosis. Most of them were obese with a BMI above 30, and most were migrants.
In Sweden, more women admitted with COVID-19 had other co-morbidities than in other Nordic countries.
Again, of the nearly 30% of these women who had multiple pregnancies, 90% were in Sweden. Finally, Swedish women tended to test positive at later terms of pregnancy and delivered earlier after the diagnosis.
Swedish cases came from tertiary care hospitals, which may account for the higher number of gestations complicated by multiple pregnancies and underlying conditions in this country. The use of universal obstetric screening on admission in one of the three Swedish hospitals included in this study may explain the lower rates of preterm and Cesarean deliveries, as cases from the other countries included only severe COVID-19 presentations during pregnancy.
Management and outcomes of COVID-19 in pregnancy
Of the 56 pregnant women hospitalized with COVID-19, 12 women required admission to an intensive care unit (ICU). None of the women died of COVID-19.
Induction of labor was somewhat more common in Sweden than in other countries, but the Cesarean delivery rate was lower, at ~39% vs 53%, respectively.
There were 49 infants born to 48 women during this period, of which ~42% were delivered by a Cesarean. This is an increased proportion compared to ~17% in 2018. Emergency Cesarean rates were also higher, at 85% vs. 54%, compared to 2018 rates.
Women with COVID-19 in pregnancy also had higher rates of preterm delivery, at 25% vs. ~6% in 2018.
Seven of the infants required admission to the neonatal ICU (NICU), but no stillbirths or infant deaths were reported. NICU admissions were lower in Sweden, at ~7%, compared to ~28% in other Nordic countries.
What are the implications?
This prospective study covers only pregnant women with the most severe forms of COVID-19, thus eliminating biases due to differential testing strategies in different countries. The findings show that the risk of hospitalization in pregnancy because of COVID-19 is low, and the outcome generally favorable.
The fact that more than a fifth of the women needed ICU admission is probably because this study included only the most severe cases. Earlier studies have indicated that pregnancy increases the risk of ICU admission for COVID-19.
Interestingly, the rates of admission were higher in Sweden than in other Nordic countries, possibly reflecting the higher rates of hospitalization and ICU admission in the population as a whole in the former region.
“This may indicate that policies reducing the transmission in the general population also reduces the rate of hospital admission due to COVID-19 among pregnant women.”
Obesity and non-Nordic origin tended to increase the risk of hospitalization. This knowledge may shape public health policies directed at lowering the risk of adverse outcomes in this group.
Women who were admitted in pregnancy because of COVID-19 were more likely to deliver preterm or by Cesarean section, in agreement with other studies that show these outcomes increase with the severity of COVID-19.
Pregnancy-related risks of adverse outcomes due to COVID-19 depend on national public health strategies and the resulting population-level transmission of the virus. International collaborative studies help evaluate less common complications and risk factors that may affect obstetric outcomes during the pandemic.
*Important Notice
medRxiv publishes preliminary scientific reports that are not peer-reviewed and, therefore, should not be regarded as conclusive, guide clinical practice/health-related behavior, or treated as established information.