Analysis reveals 63% of the COVID-19 cases in the US until August 2020 originated from people between the ages of 20–49, while about 1.2% of the cases originated from children 0–9 years old. However, this could change as schools re-open.
.jpg)
The spread of the COVID-19 pandemic caused by the severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2) since the beginning of 2020 has led to dramatic interventions to contain its spread. The virus spreads through human contact, so one of the strategies has been to limit person-to-person contact.
Several countries used near-total lockdowns and stay-at-home orders to limit personal contact. How people interact with each other has changed dramatically since these interventions. Data from the US showed the average number of contacts per person was four or less. In China, children had almost no contact with each other during the initial weeks of the lockdown and had reduced contact with older persons.
Because of such strategies, the number of cases declined during the first half of the year. But, there has been an increase in the number of cases since the middle of June in the US, with more cases also being reported in Europe.
Modeling infection spread in the US
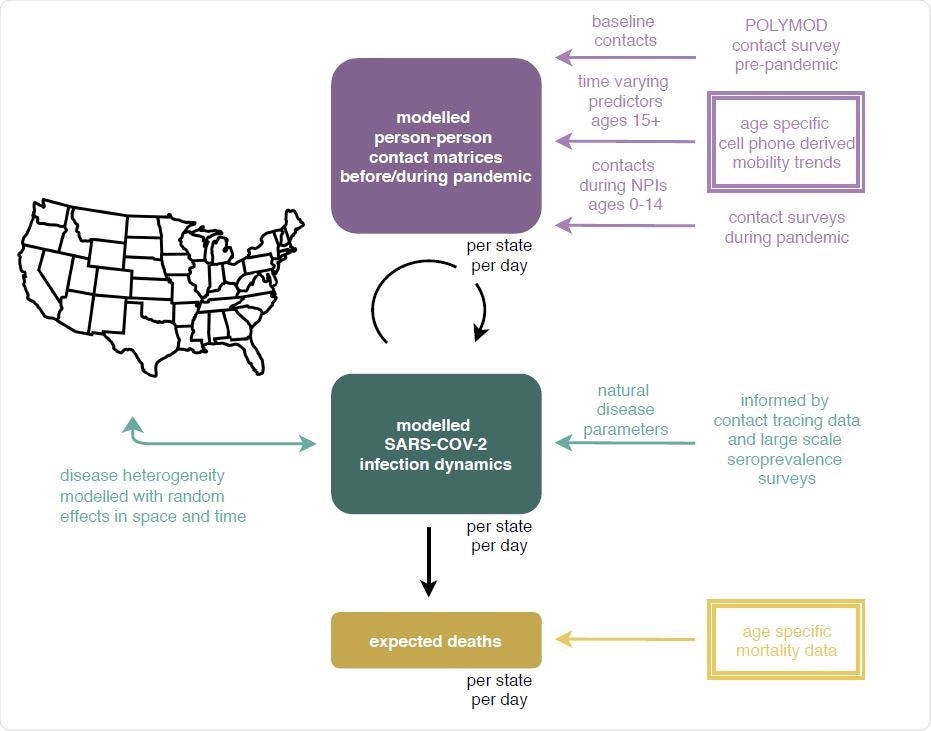
In a new study published on the preprint server medRxiv*, a team of researchers on behalf of the Imperial College London COVID-19 Response Team used longitudinal and age-specific population mobility and COVID-19 mortality data to model and predict SARS-CoV-2 spread in the US.
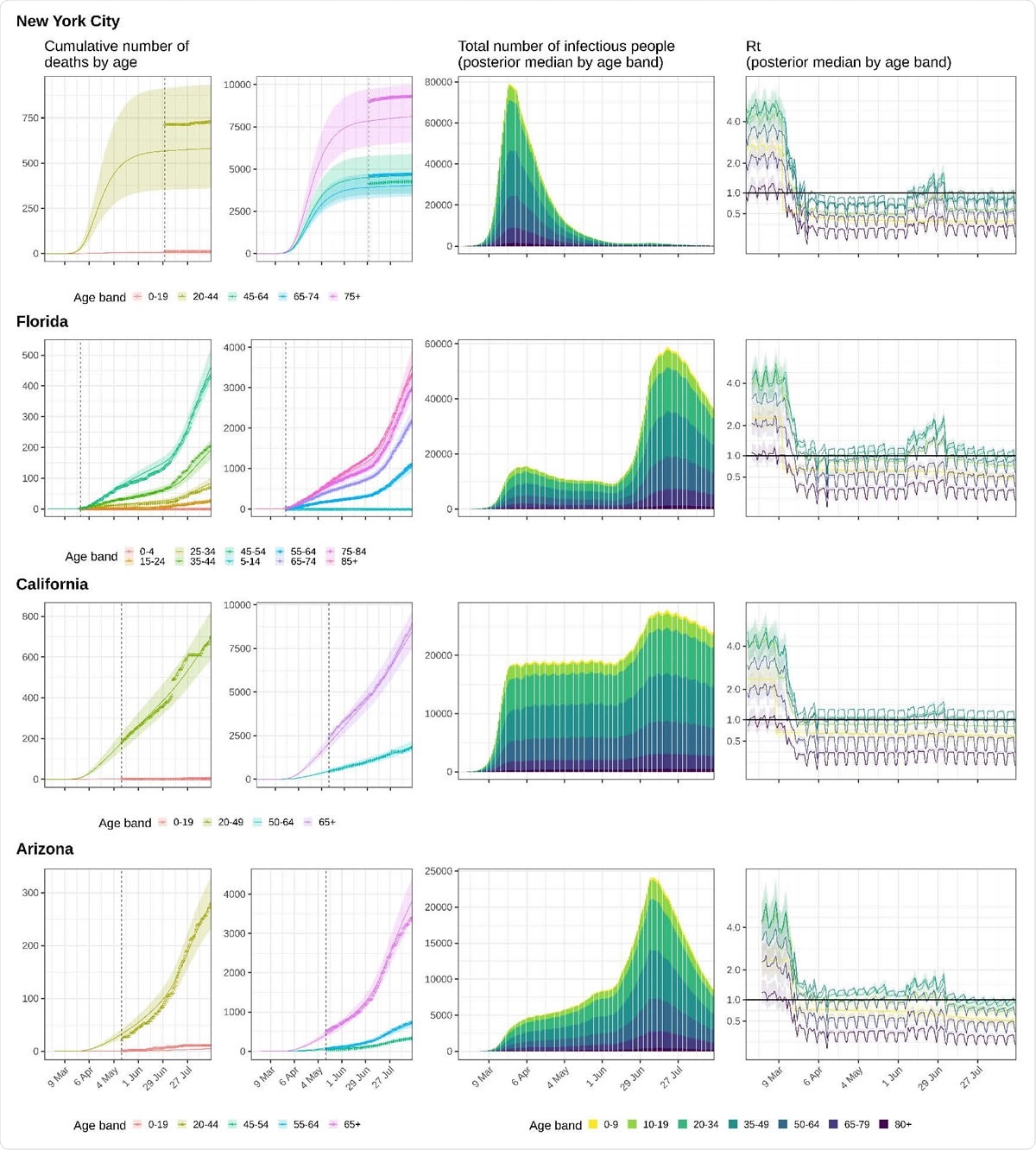
In their model, they determined contact intensities, which are the expected number of contacts made by a person, at a population level, and for specific age groups in the US. They used cell-phone data to estimate the movement of persons over 15 years to determine how to contact intensities changed during the pandemic. For children under 14 years, they used data from contact surveys conducted when schools were closed. They determined baseline contact intensities using contact survey data from before the pandemic.
Using cell phone data and Foursquare’s location technology, Pilgrim, they compiled a national-level mobility data for more than 10 million persons in the US. The technology shows user visits to different locations and time spent at a location using mobile signals. The data were aggregated by different age groups: 18–24, 25–34, 35–44, 45–54, 55–64, and 65+.
Adults drive spread
The mobility trends saw an initial decrease in visits outside the house for about a month starting the middle of March compared to levels before stay-at-home orders but gradually started increasing after the middle of April for all age groups.
For all the states evaluated, the reproduction number was consistently lowest for children 0–9 years and people over 65. By 17 August 2020, the reproduction number was above 1 only for people aged 35–49 years, contributing to about 35% of spread in the infection. People aged 20–34 contributed about 28% to cases. So, adults between 20-49 years were responsible for about 62% of the infections.
Based on their analysis, the authors believe that the mean age of new infections has remained constant, and changes in transmissions by specific age groups is not a key driver of the epidemic in the US yet.
When schools open
However, as schools re-open in the US in August and September, this could change. If children aged 0–11 years return to school and contact behavior patterns remain the same, as before the pandemic, there could be an increase of cases by about 250% by the third week of November 2020, predicts the model. This is assuming the trends for other age groups don’t change, and face masks are used.
![Predicted COVID-19-attributable deaths in the central kindergarten and elementary school reopening scenario. Posterior median estimates (line) are shown along with 95% confidence interval (shaded area). Daily COVID-19-attributable deaths as reported from [2] are overlaid (red bars). Estimated expected deaths are shown in blue for the observation period. Predicted expected deaths in the continued school closure scenario are shown in green. Predicted expected deaths in the school re-opening scenario are shown in yellow. This scenario assumes a 50% transmission reduction from and to children aged 0-11 due to face mask use and other non-pharmaceutical interventions. Predicted COVID-19-attributable deaths in the central kindergarten and elementary school reopening scenario. Posterior median estimates (line) are shown along with 95% confidence interval (shaded area). Daily COVID-19-attributable deaths as reported from [2] are overlaid (red bars). Estimated expected deaths are shown in blue for the observation period. Predicted expected deaths in the continued school closure scenario are shown in green. Predicted expected deaths in the school re-opening scenario are shown in yellow. This scenario assumes a 50% transmission reduction from and to children aged 0-11 due to face mask use and other non-pharmaceutical interventions.](https://www.news-medical.net/image.axd?picture=2020%2F9%2F%402020.09.18.20197376v1-1.jpg)
There could be an additional 12% extra deaths because of COVID-19 compared to when schools were closed. These excess deaths are predicted notably to be in areas with resurgences like Texas, California, and Florida if strategies are not implemented to reduce transmission from and to children. However, if transmission via children could be reduced by 66% or more, the model predicts no substantial increases in deaths.
The authors caution these predictions should be considered with limitations. “It is possible that we over-estimated the impact of re-opening kindergartens and elementary schools on transmission dynamics,” they write because of several limitations and assumptions used in the model.
There is limited data on contact patterns to and from children, and the authors used patterns from contact surveys in the UK and China. The predictions are for the state-level and could vary significantly at the county level. Furthermore, the model does not account for other factors such as household settings, a ley driver of transmission.
Although re-opening kindergarten and elementary schools is essential, the model predicts an increase in cases, particularly in areas with sustained community transmission from adults. Thus, interventions targeted at adults 20–49 years old could help contain the spread and help safe school re-openings.
*Important Notice
medRxiv publishes preliminary scientific reports that are not peer-reviewed and, therefore, should not be regarded as conclusive, guide clinical practice/health-related behavior, or treated as established information.
_c6274c997e714f48adbf7011cc8633e9-620x480.jpg)