The mitigation strategies implemented to curb the spread of COVID-19 appears to reduce the transmission of influenza in the United States, Australia, Chile, and South Africa. These strategies may augment influenza vaccines, especially for high-risk populations during the seasonal influenza transmission.
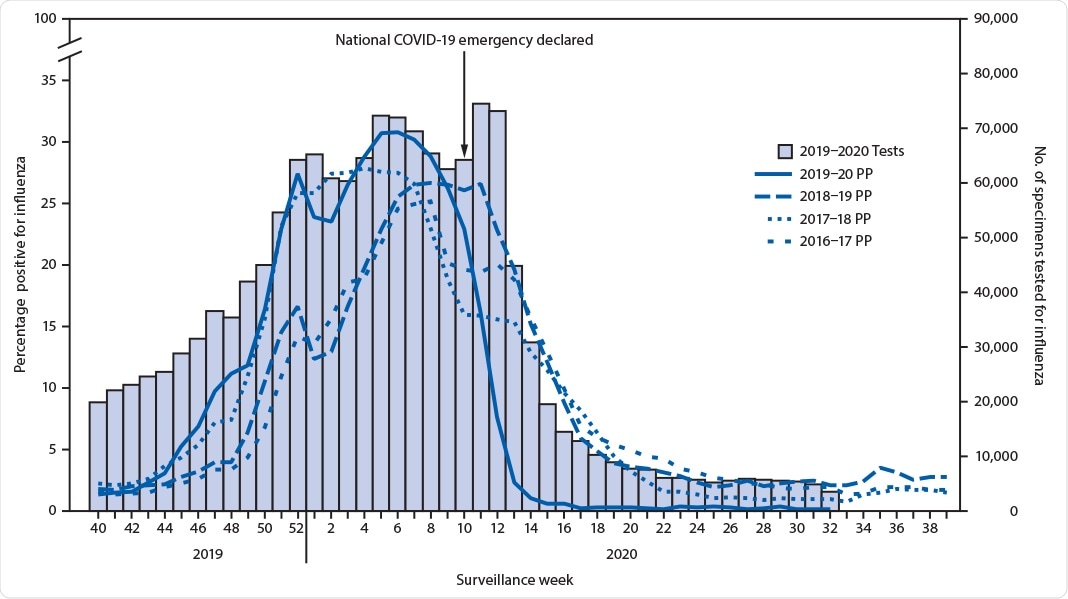
Severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2), a novel coronavirus, was first detected in Wuhan, Hubei Province, People’s Republic of China, late December 2019. Subsequently, SARS-CoV-2 spread rapidly, leading to the COVID-19 pandemic. COVID-19 is overshadowing other similar respiratory diseases such as influenza. Sonja J. Olsen, et al. report in the CDC’s Morbidity and Mortality Weekly Report that the positive influenza cases (from U.S. respiratory specimens) have dropped from >20% to 2.3% during this pandemic.
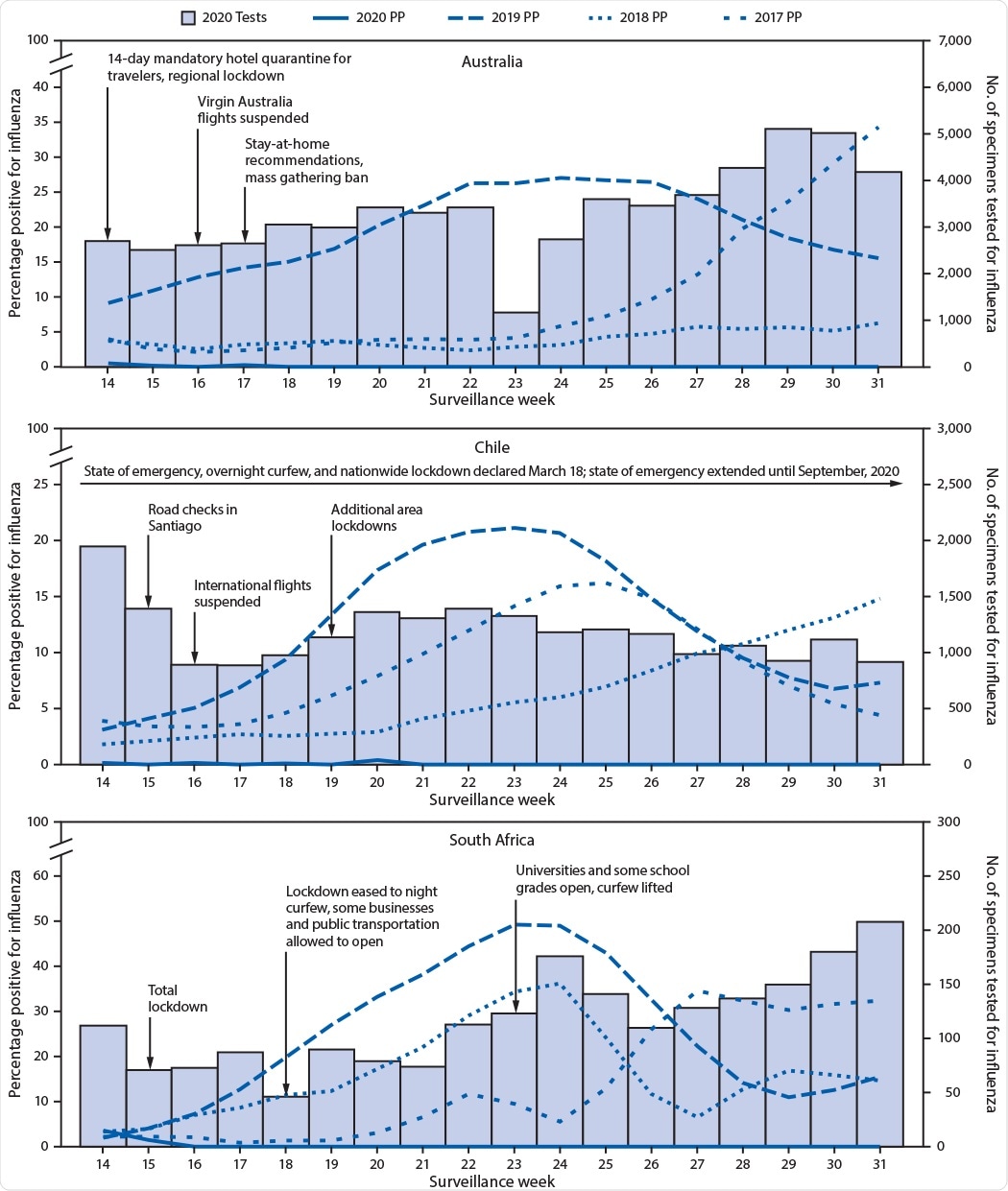
Southern Hemisphere countries also indicate the same observation, with little influenza activity. Low incidence of influenza symptoms is reported, and in those tested for influenza, few have tested positive. Interventions aimed at SARS-CoV-2 transmission, plus influenza vaccination, might be the reason behind low influenza activity in the United States and globally.
Mitigations in the face of COVID-19 pandemic included individual measures such as mask-wearing, staying home while sick, and social distancing, and community measures such as school closures, bans on mass gatherings and stay-at-home orders, and others, such as 14-day mandatory travel quarantines, national curfews, and lockdowns.
Initially, people with respiratory symptoms were preferentially tested for SARS-CoV-2. This could attribute to the observed decline in the influenza virus. However, later on, public health officials and clinicians began to test samples for influenza. Adequate numbers were tested, and little or no influenza virus was detected compared to the previous year’s incidence of influenza activity.
Australia tested more specimens for influenza, typically when the Southern Hemisphere influenza epidemics peak. They also detected only a few positive results, notwithstanding low stringent criteria for testing respiratory specimens compared to previous seasons.
While the Southern Hemisphere temperate climates have virtually no influenza virus circulation, it is observed to decline in the United States, in other Northern Hemisphere countries, and the tropics.
The decline in influenza can be due to a reduction in people seeking or reporting for respiratory illness as well as changes in the circulation of the influenza virus. The influenza virus (Ro = 1.28) is low compared with that of SARS-CoV-2 (R0 = 2–3.5). Therefore, even though influenza is also transmitted primarily by droplets, just like SARS-CoV-2, the mitigation measures adopted during this pandemic period has substantially reduced the influenza transmission.
Significance of the report
Populations at high risk for developing severe disease and complications due to influenza may continue to adapt the mitigation measures during the influenza season in addition to taking the influenza vaccine. This may be useful for high risk-prone and old-aged people, and also reduce the burden on medical care support.
The authors agree it is difficult to separate the effect of the overall mitigation measures on the influenza transmission during this season. For example, school children spread influenza, and closure of schools may effectively reduce influenza spread. However, because adults have other exposures, it cannot demonstrate the effectiveness of influenza transmission this season.
According to the authors, the findings in this report has at least four limitations:
- Although findings across multiple countries are consistent and compelling – an ecologic analysis cannot tell the causation;
- A sharp decline in global travel and increased use of influenza vaccinations – factors not taken into consideration in this study – may play an important role in reducing influenza
- Virus interference: this might help explain the lack of influenza during a pandemic caused by another respiratory virus that might outcompete influenza in the respiratory tract
- It is also possible that the decline in influenza observed in the United States is just a natural end to the influenza season. However, post-March-1 2020 (declaration of a national emergency related to COVID-19), a sharp decline in influenza-positive cases was observed.
Influenza spread is still being monitored to find if the low-level activity persists even after the mitigation measures are dropped. However, under the current uncertain circumstances, it is vital to plan and prepare for seasonal influenza circulation, especially in the 2020–21 Northern Hemisphere season. Additionally, a new Food and Drug Administration (FDA) – approved multiplex diagnostic assay for detection of both SARS-CoV-2 and influenza viruses could improve the predictive efforts and also direct our mitigation strategies for both the diseases.
With the impending fact that this season the SARS-CoV-2 and the influenza virus might cocirculate, the best method for influenza prevention is influenza vaccination (for all persons aged ≥6 months). Keeping the limitations in mind, the authors conclude that the widespread implementation of measures to mitigate transmission of SARS-CoV-2 is associated with the decline in influenza incidence – which appears to be real and concurrent with the COVID-19 pandemic.
- Olsen SJ, Azziz-Baumgartner E, Budd AP, et al. Decreased Influenza Activity During the COVID-19 Pandemic — United States, Australia, Chile, and South Africa, 2020. MMWR Morb Mortal Wkly Rep 2020;69:1305–1309. DOI: http://dx.doi.org/10.15585/mmwr.mm6937a6