The COVID-19 pandemic caused the closure of many schools around the world, both primary and secondary, in March or April. This has been estimated by different researchers to have widely varying impacts on the incidence and mortality of COVID-19. For instance, one study shows that weekly incidence was reduced by 62%, and weekly deaths by 58%, while others estimated only a 2% to 4% reduction in deaths.
Now a new study by researchers at the Institute for Disease Modeling and published on the preprint server medRxiv* in September 2020 focuses on modeling the potential risk of COVID-19 for school students and staff if schools are re-opened in a range of scenarios. This could guide further research on the health and educational outcomes of school reopenings.
Risks and Benefits
Public educational experts assert that learning in school has many benefits for the child, whether in terms of social interactions, physical play, and activity, or educational resources. In children from poverty-stricken families, a school may make the difference in eating or going hungry. In keeping with this perception, the American Academy of Pediatrics supports the re-opening of schools.
The researchers point out that this will also put almost one in four teachers at higher risk of falling gravely ill due to COVID-19. In fact, almost 80% of teachers in one US poll in July said they were concerned about the risk to their health once schools re-opened, and two-thirds said they would prefer remote learning to continue.
In Europe and Asia, the school re-opening experience has varied. Some opened smoothly, and others closed almost as soon as they re-opened because of a spurt in outbreaks within schools. Most countries initiated reopenings when the case detection rate over the preceding 14 days was less than 25/100,000. In many cases, younger students were first returned to in-person learning, and schedules were switched around to enable some cohorting.
Risk Reducing Behavior
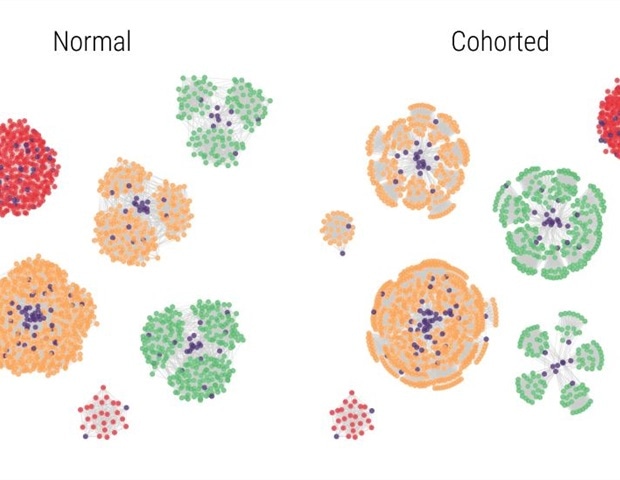
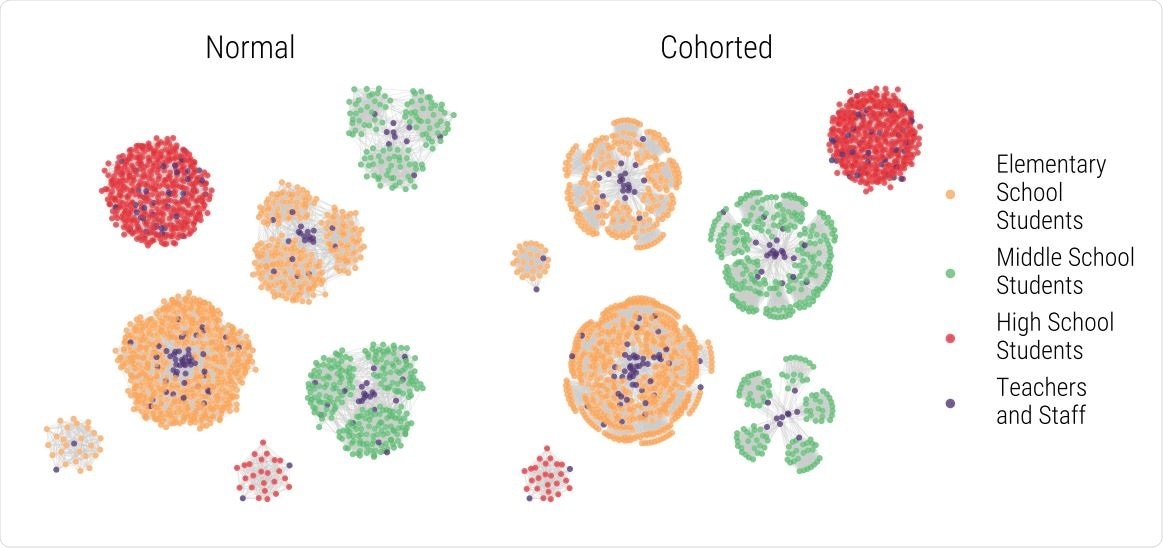
The current study focused on finding the impact of behavioral changes such as mask-wearing, physical distancing, hand hygiene (all three together may reduce transmission by a fourth), case detection (by screening any symptomatic person, diagnostic testing of positive screens, and tracing contacts), and changing classroom structure (creating cohorts of students and teachers which reduces contact with others outside the classroom, changing the schedules to A/B patterns where alternate groups of children who attend on different days of the week, and switching between remote and in-person classes).
Assumptions and Scenarios for Re-opening
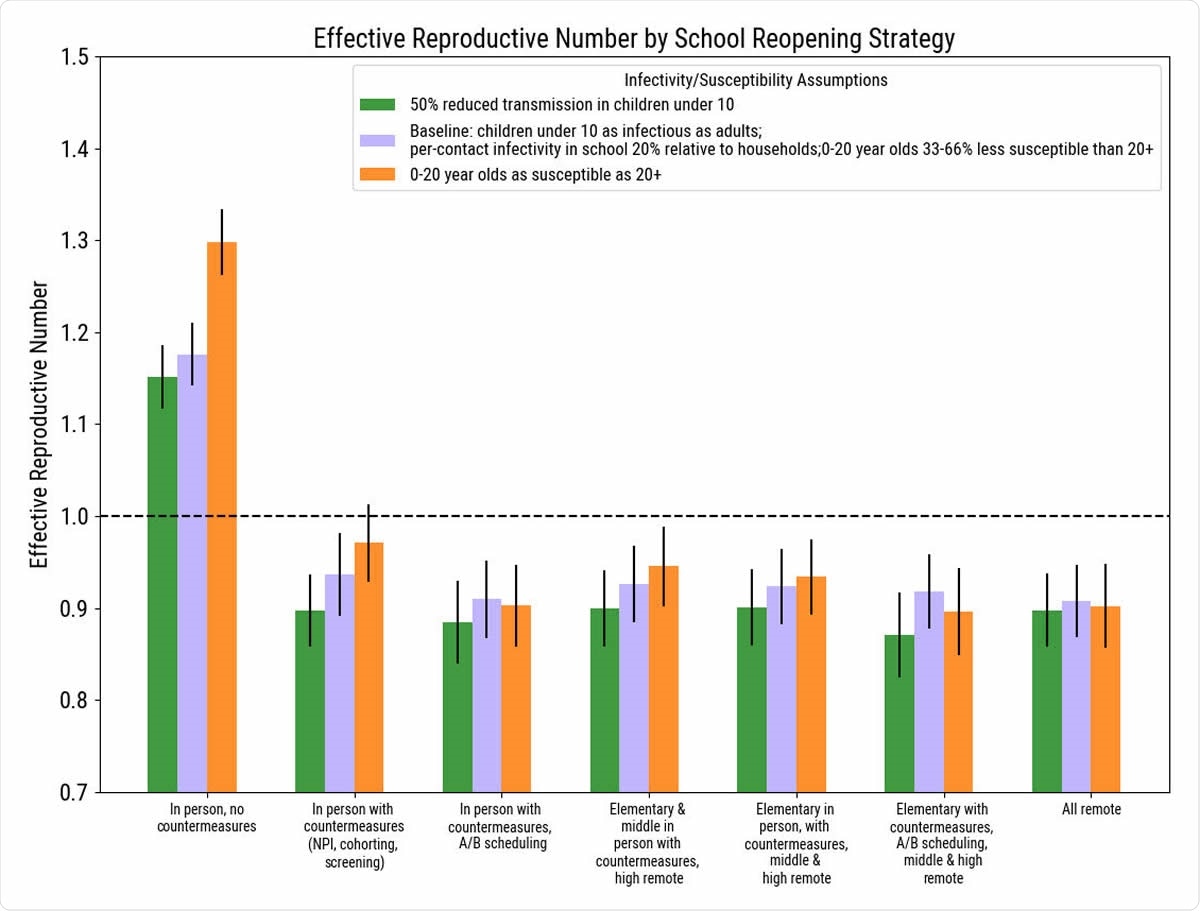
The researchers looked at seven scenarios, depending on the level of countermeasures used at school, from none to all, and from only elementary school to both elementary and middle school in-person learning, and from simultaneously schedules to A/B scheduling, or completely remote learning.
The assumption was that preschools and universities would not open and that high schools would be unable to apply separate cohorts for students given the highly individualized schedules at this level. They modeled the first three months of the school term, defining average class sizes and the number of students per school.
The researchers used the effective reproduction number Re, well as the case detection rate in the two weeks before schools re-opened, to indicate the size and the trajectory of the outbreak in that region. They assumed that with schools closed, the epidemic was slowly waning, with an Re of 0.9. They estimated school-based transmission for case detection rates of 20, 50, or 110 diagnosed cases per 100,000 individuals, fitting the definition of low, medium, and high case detection rates in the US concerning school re-opening.
They concluded, “In-person schooling, even with sufficient countermeasures, poses significant risks to students, teachers, and staff.”
Impact of Various Measures
The model shows that at least one COVID-19 case would show up at school in anywhere from 5% to 42% of schools. Asymptomatic infections will go unmarked. Symptomatic individuals will be detected by screening and sent home.
The model also shows that without school countermeasures, with a high case detection rate, almost 25% and 20% of staff/teachers and students respectively will come to school while carrying the infectious virus. If re-opening is delayed until the case detection rate is 20/100,000, this risk is reduced by 2.5 times.
All active infections may not be equally infectious, and school countermeasures will play a significant role in minimizing the risk of onward spread. These include case detection, isolation, contact tracing, and quarantine. If these are in place, the reduction in incidence will be four-fold less even at the highest case detection rate.
Using A/B schedules would still further reduce the risk of viral spread, especially if only elementary schools are re-opened.
In such a situation, the cumulative infection rate could be as low as 0.2% to 1.7%, and 0.1% to 1%, for staff and students, respectively.
“This represents,” they say, “at least a 14-fold reduction in the risk of COVID-19 for teachers and staff in schools,” compared to universal re-opening without countermeasures.
For instance, for a county with a population of 2.25 million, this would mean 900-6,200 more tests in the first three months of school.
Conversely, if an A/B approach with two groups per classroom attending two days a week in staggered fashion is used, the viral spread would be only about 0.6 – 4.3% and 0.4 – 3.1% for teachers/staff and students, respectively. It may be observed that this is higher than the risk with the first scenario, but it offers all the students in the school some opportunity to attend school.
Will School Reopening Also Increase Community Spread?
The researchers also estimated that in order to minimize infection rates within schools, about 83% of learning days would have to be at home, either because of COVID-19 related measures like quarantine or isolation or because of remote learning.
The most significant effect, however, is because of the pre-opening COVID-19 infection rate and not the school strategy, since if the population prevalence is high, the infection rate is seven times higher than if it is at the lowest level. Moreover, under the assumptions that the researchers operated on, community transmission is unlikely to increase much as long as schools take precautions during re-opening, and the latter occurs at a time when community spread is decreasing.
While the current study assumes that children from K1-12 are as infectious as adults, other studies have indicated that children under 10 are half as infectious. Susceptibility-wise, it is assumed that below the age of 10 years, children are only a third as susceptible as older adults, while for those between 10 and 20 years, it is two-thirds that of older adults. This may not be the case, according to a recent pediatric study in Australia, which suggests that they are equally vulnerable. However, this is unimportant, provided countermeasures are taken in schools.
Implications and Future Directions
The researchers conclude that, with respect to in-person learning, “Modeling results suggest that, depending on the case detection rate of COVID-19 in the community, an incremental approach that returns the youngest students first with a reduced schedule would minimize the risk of infection within schools and provide important benefits to the neediest children.’
Returning the youngest students who have the lowest susceptibility first, therefore, has the highest risk-benefit ratio. Some countries have done this with a lower incidence rate at the time of re-opening. The case detection rate and the size of the school will determine which strategy is optimal.
Secondly, the most significant reduction in risk costs the greatest in terms of loss of in-person learning days. Remote learning has widely varying benefits depending on the age, economic and social status, and the resources available at home. Even when this is adopted, screening of symptomatic individuals with quick isolation, contact tracing, and quarantine will be essential to reducing the risk of transmission.
The study is limited by the many assumptions, based on the literature, and the omission of contacts at the workplace by parents after schools re-open. The increased burden of contact tracing on local healthcare efforts is not included in the analysis. Moreover, the contacts made between children out of school and during transportation, as well as the difficulties in creating cohorts with limited resources and highly variable elective courses, are omitted. Thus, further refinements are required to estimate the impact of school opening on viral transmission.
Nonetheless, the study shows, “Re-opening schools is not a zero-risk activity.” The challenge ahead is to balance the risks to the teachers and staff with the benefits to the students while treating COVID as the community problem it really is.
*Important Notice
medRxiv publishes preliminary scientific reports that are not peer-reviewed and, therefore, should not be regarded as conclusive, guide clinical practice/health-related behavior, or treated as established information.