The spread of the ongoing COVID-19 pandemic has spared neither male nor female, old nor young, and many pregnant women have fallen victim to it as well. However, the impact of this infection on the pregnant mother and the baby are as yet uncharacterized.
Now, a new study published on the preprint server medRxiv* in July 2020 reveals evidence of placental infection and hypoxia, despite the lack of serious symptoms in the mother. This could indicate the need for a more rigorous analysis of possible fetal hypoxic damage in future research, as well as helping to shape policy guidelines in pregnant women.
.jpg)
The Study: Normal Pregnancy Outcomes with COVID-19
The current study deals with a pregnant woman aged 29 years, a multigravida, admitted past 40 weeks for induction of labor. She had experienced muscle pain a couple of days prior to presentation and was tested for severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2) by reverse transcriptase-polymerase chain reaction (RT-PCR), which was positive.
The patient’s parents were known to be positive for the infection. They were self-isolating, while her husband had been in contact with a workplace outbreak but tested negative and was asymptomatic for the disease.
The pregnancy had been uncomplicated so far, and the patient remained healthy throughout pregnancy, with normal muscle pain being relieved before admission. She delivered a baby boy weighing about 3,500 g. Both mother and baby were discharged 36 hours from birth. At 24 hours post-birth, the RT-PCR was negative for the baby, and at one week, the infant was breastfeeding normally without any symptoms suggestive of COVID-19.
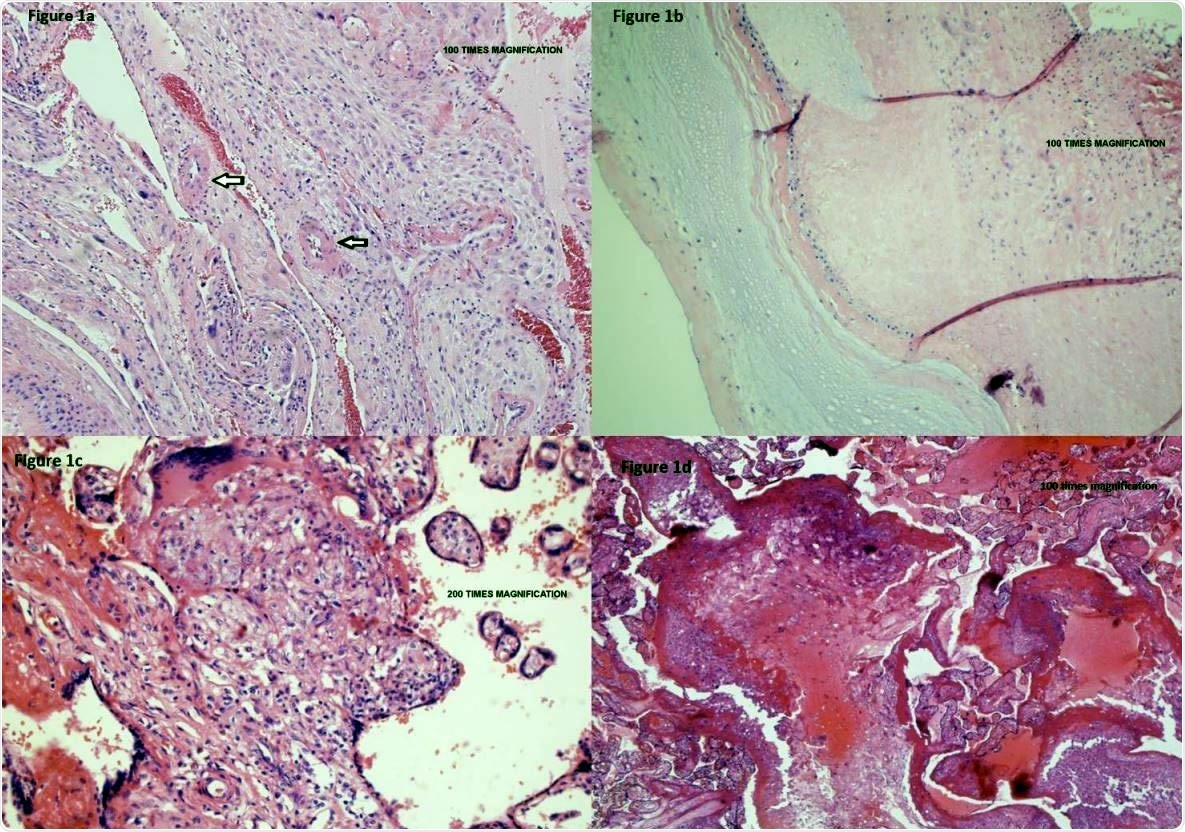
Abnormal Placental Histopathology
Histopathological examination of the placenta showed evidence of acute uterine hypoxia as shown by subchorionic laminar necrosis, with underlying chronic uterine hypoxia, shown by extravillous trophoblasts and focal chronic villitis. Immunohistochemistry (IHC) analysis showed the presence of SARS-CoV-2 antigens extensively distributed throughout the placenta. These were present under the umbilical cord, in both central and peripheral placenta, in the endothelial cells of the chorionic villi, and uncommonly within trophoblasts.
Prior Research on COVID-19 IN Pregnancy
Until now, the 12 case series published in COVID-19 literature with respect to this disease in pregnancy report that severe COVID-19 is not typical in pregnancy. In fact, out of 431 cases, 36 had a serious or critical disease and required ICU admission. Other studies have confirmed the low risk in pregnancy.
However, two studies, one from Sweden and one from the USA, indicate a less rosy picture. In the first, the risk of ICU admission was fivefold, and the risk of mechanical ventilation fourfold, relative to nonpregnant women, four times higher.
In the US study, carried out on almost 330,000 women in the reproductive years who were positive for COVID-19, they found that pregnant women were about 50% more likely to be admitted to the ICU, and 70% more likely to receive mechanical ventilation. This comes to an absolute risk of 1.5% that pregnant women will need ICU care. Overall, the maternal mortality is 0.2% from this disease.
The Traces of COVID-19 in the Placenta
Vertical transmission from mother to fetus also appears to be low, but several reports have shown the presence of the virus on fetal membranes. In the placenta, COVID-19 is thought to infect the endothelial cells leading to a procoagulable state.
This can cause microthrombi to form, which in turn can cause inadequate perfusion of the blood flow through the placenta. This is evidenced by accelerated villous maturation, infarction, intervillous thrombi, lesions of extravillous trophoblast, and subchorionic laminar necrosis.
The effect on the fetal circulation is reflected by clots within the larger vessels, villous sclerosis, and breakdown of the endothelial cells within the villous stroma. A placental study showed impaired perfusion from the fetal side in 8/20, and maternal side in 3/20 placentas. Another study showed that placentas of COVID-19 patients were commonly marked by decidual arteriopathy and intervillous thrombi.
The important thing is that the signs of fetal and maternal malperfusion are not specific for COVID-19, being seen in other hypercoagulable states like lupus anticoagulant, protein C or S deficiency, gestational hypertension and pre-eclampsia, or even in otherwise normal pregnancies.
Current Recommendations for Pregnant Patients
The continuing surge in COVID-19 cases in the USA has caused a great deal of concern about the possibility of viral mutations. In accordance with its earlier report, the Center for Disease Control (CDC) published recent recommendations about pregnancy in COVID-19.
These include recommendations to stay away from others as much as possible, to protect oneself against COVID-19 in case of unavoidable interactions, and also a warning that some babies have tested positive for the virus. However, the timing of infection remains unclear.
Placental Infection in Mild Maternal COVID-19
The current paper is the first to describe the results of IHC of placental tissue from women with mild COVID-19, though there are six which report the presence of the virus in the placentas of women with moderate to severe disease. The patient in this study had no fever, cough, or shortness of breath, typical symptoms of the infection.
She did have a history of contact with sick people and myalgias. Even so, the placental tissue showed the possibility of vascular involvement. This is among the most serious of placental issues since it can lead to fetal growth restriction, pre-eclampsia, and vertical transmission if the mother is infected in early pregnancy.
The current paper describes that the virus made its way across the placenta and the presence of placental vascular disturbances. This resulted in poor perfusion on the maternal side of the placenta, with lesions of the extravillous trophoblast and subchorionic laminar necrosis.
However, fetal malperfusion was not seen. Despite the presence of SARS-CoV-2 in the placenta, the virus was absent in the newborn. This is not a generalizable finding since the woman tested positive for the virus later in pregnancy. Early or multiple exposures could have different effects. This will require more research, including these specific conditions.
Implications
The study concludes: “Evidence of placental COVID-19 raises concern for placental vasculopathy and potential vertical transmission. Our report raises the question of whether future pregnancy guidance should include even stricter pandemic precautions, such as prenatal screening for a wider array of COVID-19 symptoms, increased antenatal surveillance recommendations, and possibly COVID-19 testing on a regular basis throughout pregnancy.”
*Important Notice
medRxiv publishes preliminary scientific reports that are not peer-reviewed and, therefore, should not be regarded as conclusive, guide clinical practice/health-related behavior, or treated as established information.
_e081922bd08c4976b0ec52b03e525f5a-620x480.jpg)